Interview: Colonoscopy is a disease prevention
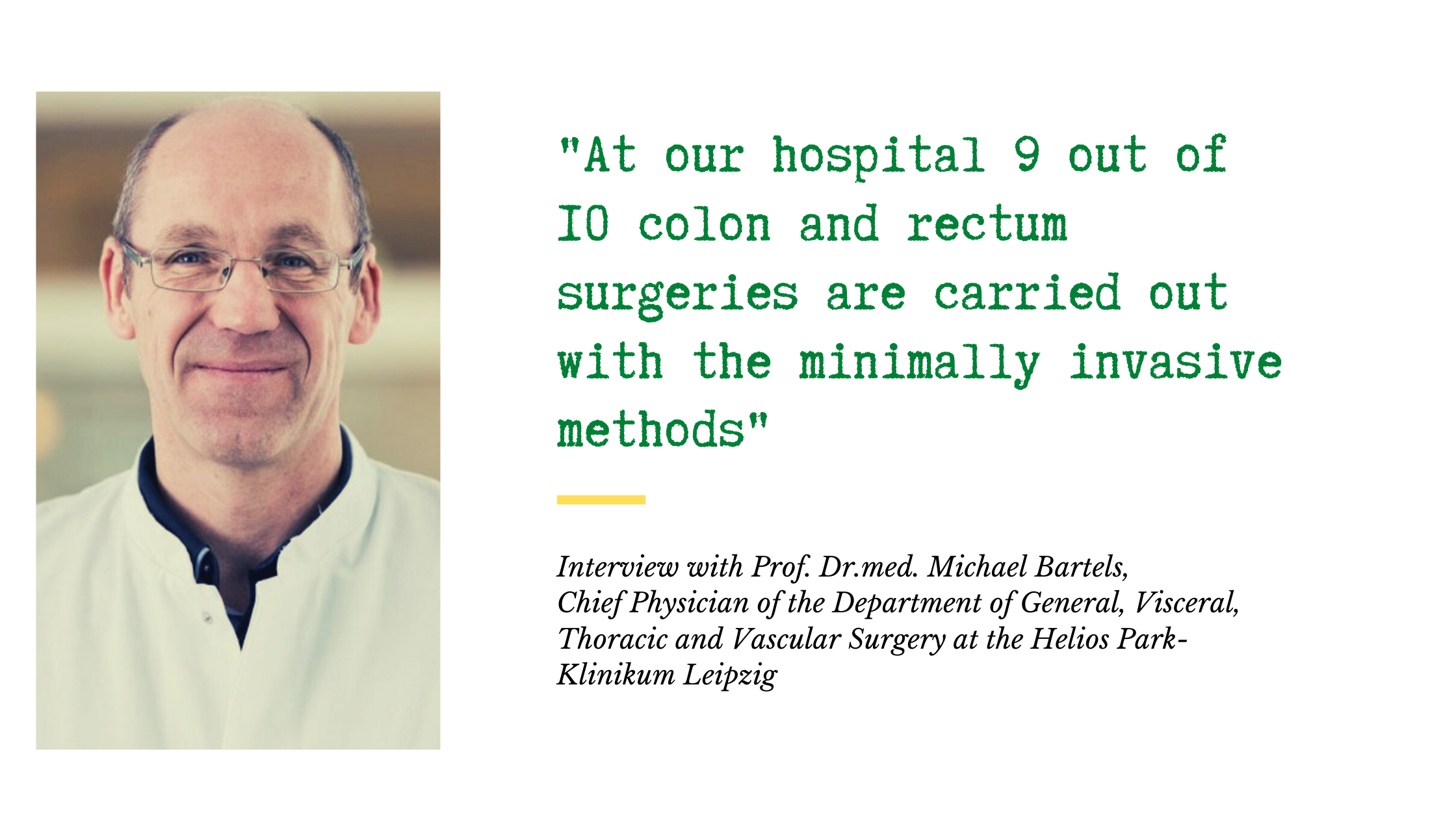
Prof. Dr.med. Michael Bartels, the chief physician of the General, Visceral, Thoracic and Vascular Surgery at the Helios Park Hospital Leipzig, answers the patients’ questions about colon, liver and pancreatic cancer.
Obesity and too much fatty and unhealthy food are often to blame. We also see a connection to a lack of physical activity, however there has not been enough research done on the subject. There are genetic factors as well-meaning, that if you have a relative, especially a parent, a sibling or a distant family member who has been diagnosed with cancer at a young age, you should do a regular check up from age 45, otherwise, after age 55.
We should distinguish between a prevention and averting. Colonoscopy is a preventive measure, which means that we can detect a tumor before the symptoms show. The alternative would be a fecal occult blood test and a CT-guided virtual colonoscopy. However, it’s far from being as precise as a traditional colonoscopy.
Yet, a colonoscopy is not only a preventive measure, but also a method to avert a disease. This exam can detect warning signs of cancer – polyps. They are usually very small, about one cm in diameter, and don’t cause any symptoms. In that regard, we can’t substitute a colonoscopy, because a CT often doesn’t show polyps at all.
Yes, it’s the only way. As soon as we detect a polyp, we remove them right away in order to avert the development of early stages of cancer.
It’s a good question, which doesn’t have an exact answer. It might be possible. There is a certain sequence, which is a polyp, an adenoma, a carcinoma. Can a cancer skip the first two stages? When we discover a carcinoma, it is already impossible to rewind to find that out.
Sometimes we need to open the abdomen to remove a tumor. Therefore, there are some patients, who think that if air gets into the stomach, it will explode.
It is indeed a risk factor. We do not have a statistical proof yet, but there is a correlation between red meat and a colorectal cancer. To reduce the risk, you should stick to a healthy diet. Try eating lots of vegetables and fruits and cut down the meat. Be careful not to put on excess weight and work out more. However, even employing all these measures will not guarantee 100 % safety. There are thin people who exercise regularly and eat healthy, all while coping with cancer. Thus, the most important thing is a preventive check up.
They are actually the same. Obesity and unhealthy diet cause metabolic syndrome followed by fatty liver, also known as steatosis, which might lead to liver cancer. Another reason would be alcohol consumption and liver cirrhosis. Therefore, if you avoid fatty food and alcohol, you might significantly reduce the risks of getting liver cancer.
Not really. Stomach cancer is rarely caused by nutrition: more often, it develops without any obvious reason. Maybe spicy food and alcohol might play a small part. However, alcohol and smoking are accountable for all types of cancer.
You explained the importance of prevention. How often do you encounter advanced cases?
They are not rare. For example, many young patients from Russia already have late-stage cancer. Sometimes those patients had symptoms but didn’t see a doctor anyway. I can’t explain why this is happening to my Russian patients, it’s just my observation.
The most widespread type of colon cancer is a tumor in the upper part of colon. We usually treat these patients with minimally invasive methods and then conduct chemotherapy. If we deal with rectal carcinoma, a radiotherapy and chemotherapy are carried out prior to the surgery, which is then followed by another chemotherapy.
During a minimally invasive procedure, we operate on the patient with a camera and tools that are inserted through special blood vessels. A surgeon makes only 4 to 5 small incisions, each measuring about 1 cm, and one bigger incision in the abdomen, which is used as an exit hole for a removed part of the colon or liver. The recovery period after such surgery is shorter and the complication risks are significantly lower.
Minimally invasive procedures are a gold standard when treating colon and rectum carcinoma. At our hospital 9 out of 10 colon and rectum surgeries are carried out with the minimally invasive methods. Sometimes it’s impossible due to a lot of reasons, e.g. if a tumor is too big, or if a patient already had a surgery done.
With liver cancer, the possibilities of minimally invasive procedures are limited. If a surgery is extensive and complicated, a minimally invasive procedure will not necessarily make it easier and faster.
Considering stomach surgery, more and more procedures are minimally invasive. It’s a promising area with a lot of room to grow, so we are trying to keep up with constant developments and sometimes even pioneer the new methods.
Patients with colon cancer and many patients with liver cancer only benefit from a minimally invasive procedure. The stomach surgeons are working towards the same results. However, the situation with the pancreas is different.
First, the pancreatic tumors can be quite large, so they can’t be operated with minimally invasive methods. Secondly, even when it is possible, a minimally invasive procedure would take twice as much as open surgery, which isn’t doing the patient any good. At the end of the day all that matters is an accurate removal of a tumor, while trying our best not to risk the patient’s life. Pancreatic tumors are handled better through an open surgery. That’s why the education and expertise of a surgeon regarding not only minimally invasive but also open surgeries are of great importance. A surgeon should master both fields and develop an individual strategy for each oncological patient.
Cancer treatment became very holistic, there are many steps. One doctor cannot possibly cover everything, that’s why several physicians should be involved in the treatment, including a surgeon, a gastroenterologist, an oncologist, a pathologist, a radiologist and a radio therapist. Everybody should have a saying in a joint therapy planning.
Exactly. During this meeting, we present and discuss cases with all colleagues. It’s a strict and important rule.
We gather once a week with a list of patients and go through these cases in alphabetical order. Radiologists also look at the X-ray images. All together, we go over kinds of therapies and their order for each patient and at the same time have everything written down. All the decisions are documented and entered in the database.
I cooperate with my colleagues from the experimental pathology – they conduct tissue research. These are not doctors, but scientists. I engage in constant collaboration in this field in order to level up the expertise of the whole department, not only from medical, but also from scientific point of view.
A university doctor is a far more well-educated and experienced specialist in many areas. Besides, a university hospital is a place for hard work. It is difficult to keep up with education and work at the same time, one requires a certain stamina. Some people have it, others – don’t.
About 40 – 50.
I usually attend to the most difficult cases and almost all cases concerning pancreas. However, I am always present at the surgeries of Russian patients, whatever the type of procedure is.
I had a Russian patient from Russian Volga Federal District. She had a rectum carcinoma and huge metastases in the liver. My colleagues in Russia defined her cases as inoperable. When she arrived, we started with neoadjuvant chemotherapy to reduce the tumor and improve the situation. Then we performed a liver surgery. We removed a right liver segment, but there were still metastases in the left one, which at the end were removed with microwave ablation. It means that microwaves were directed at the metastases through needles to burn them. The patient returned home afterwards, but came back to go through a rectum surgery. The tumor sat really deep, and it was extremely hard to reach it, so we extracted the whole rectum and made an artificial tube for a digestive tract (colostomy).
It was challenging indeed. First of all, because it was a young and nice patient, she was only 68 years old. However, she met all the challenges courageously. Now, a year later, she lives peacefully without relapses. In such cases a patient and a doctor need a little bit of luck.
When we were talking to her with the help of an interpreter and Google, we all thought to ourselves, what a shame that we don’t speak the same language!
We perform many difficult surgeries; however, the most challenging ones are the ones that involve liver segment removal. The most difficult case was a patient with an Echinococcus multilocularis, a tapeworm found mainly in foxes, and a liver lesion. I could say no, I’m not going to do it, it’s too risky. Nevertheless, if you keep on trying going until the end, you’ll make it. It’s a great success that goes hand in hand with high risk, this is why you need to find the right balance. That is what I’ve been taught – push your limits, but no overdoing and no damaging.
At the beginning of my career, I had to work a lot more and always stayed behind extra hours. To leave work at 6 pm was like going home after lunch. Back then, we didn’t have any work hours regulation. However, it doesn’t apply to me now, only to my colleagues.
If you want to do surgery, you need to be strong, tough and very persistent.
Read more:
Do you need more information about Helios Hospitals or want to schedule your treatment?