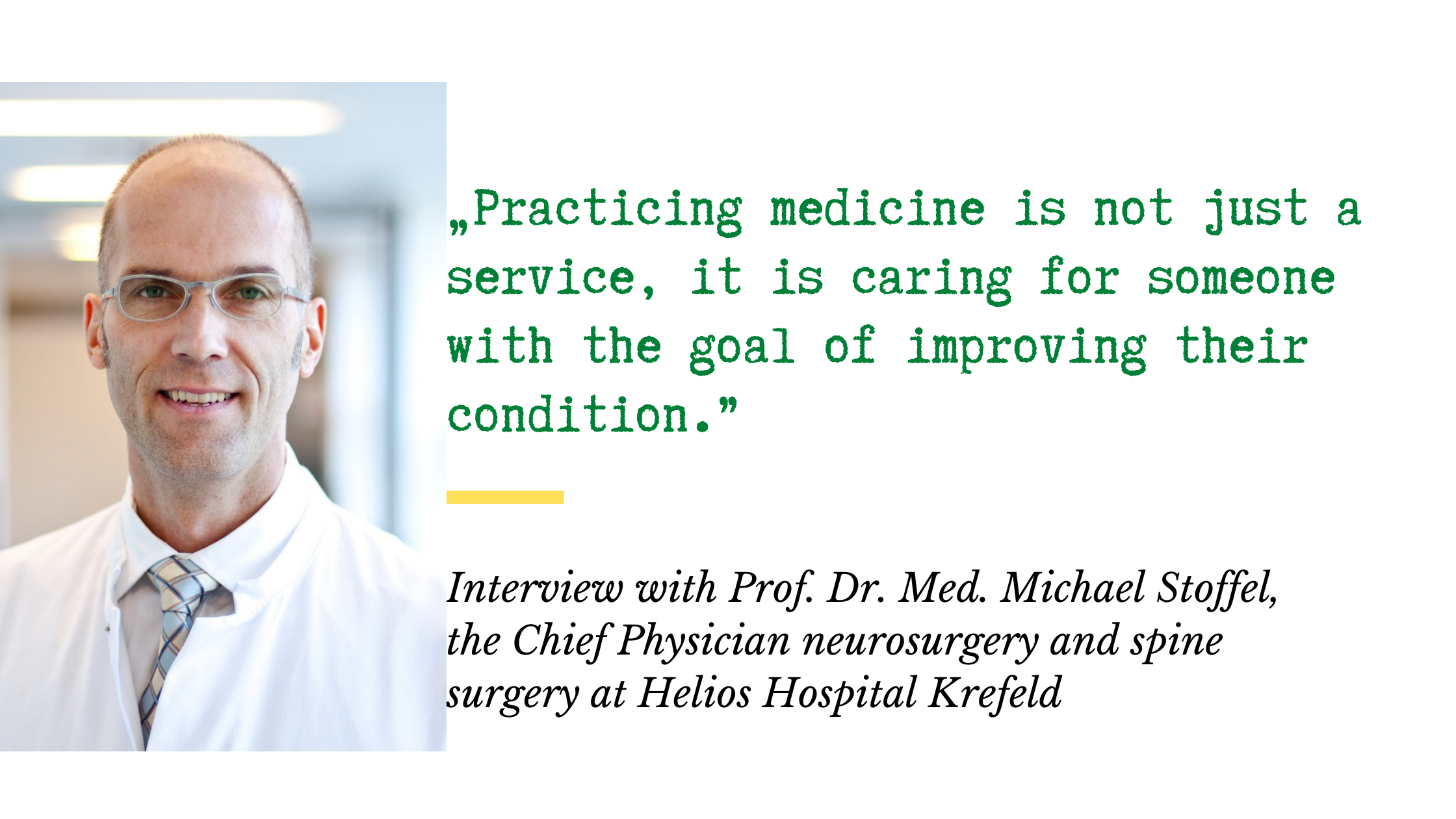
Interview with Prof. Michael Stoffel: Neurosurgery and Spine Surgery in Krefeld
Today we are talking to Prof. Dr. med. Michael Stoffel, head of the clinic for neurosurgery and spine surgery at Helios Hospital Krefeld, about neurosurgical procedures, modern surgical techniques as well as advancements in neurooncological surgery.
There is already a lot of information about the prevention of cancers such as breast or colorectal cancer, and there is a consensus in the medical community about the prevention of these diseases. This is not the case in neuro-oncology. Are there preventive measures for neuro-oncology diseases? Are there certain risk factors to look out for?
Prof. Dr. med. Stoffel: You probably think of prevention as something like not smoking, drinking little alcohol, avoiding obesity. These habits have a very general and multifaceted impact on our health with no clear, specific impact on the development of intracranial tumors. But it has been repeatedly suspected that cell phone radiation could be a possible influencing factor for neuro-oncological tumors, such as vestibular schwannomas. This has been investigated scientifically again and again, but has not yet been clearly proven. Nevertheless: In the meantime, cell phone providers recommend that you should keep your cell phone at least 1 - 1.5 m away from your head at night and that you should not make longer phone calls with the cell phone directly to your ear, etc.
You and your team perform about 1,800 neurosurgical procedures per year. How often do you personally operate?
Prof. Dr. med. Stoffel: I myself operate on about 200-250 patients as a first-time surgeon per year.
Prof. Dr. med. Stoffel: The word minimally invasive has different meanings depending on which organ you are working on. In the spine, the word minimally invasive is often used in connection with degenerative spinal diseases, and there you mean the smallest possible tissue-sparing approach to open up the muscles, the ligaments, the joint capsules as little as possible, with the goal of causing as little additional damage, instability and pain as possible. So minimally invasive is an integral part of modern spine surgery.
When thinking of the brain or spinal cord, minimally invasive primarily means how to access through the CNS (central nervous system) as gently as possible in order to achieve one's surgical goal at the end of surgery as optimally as possible while preserving function as completely as possible There is an old adage in prioritization in brain surgery and that is: "Saw bone, save brain", which means "Saw the bone" and in doing so, the access through the bone does not necessarily have to be the smallest possible, but with this goal one should achieve "save brain", that is, protect brain functions as much as possible.
Prof. Dr. med. Stoffel: First, as always, it is important to choose the most optimal approach, which in this case means the approach with the least corridor damage (to the spinal cord, but also to bones, muscles and soft tissues) on the way to the tumor - e.g., through the nose with an endoscope, through the chest cavity, through the retroperitoneal space, even through two dural layers if necessary, etc. This is a very important point. Then, of course, it requires sufficient experience in all microsurgical techniques.
Nowadays, it is also of great importance in spinal cord surgery to electrophysiologically control the function of the most essential fiber tracts of the spinal cord during surgery. This is called - as explained earlier for brain surgery - "intraoperative neuromonitoring". This is an important basic prerequisite for being able to remove spinal cord tumors safely and as radically as possible.
Then there are other tools, such as fluorescence microscopy, which typically plays a minor role in spinal cord tumors, but which we also have available. Ultimately, another important point to decide is whether, depending on which approach you had to take, at the end of the surgery the spine is still viable or whether you also have to use stabilization techniques for the spine at the end of the surgery.
Prof. Dr. med. Stoffel: For example, skull base tumors that are directly attached or partially firmly adhered to important structures that run at the base of the skull: to the optic nerves, to the optic nerve junction, to the anterior or posterior brain-supplying arteries (the carotids) or the vertebral arteries, to cranial nerves or even to essential parts of the brain, e.g. the brain stem or the brain stem vessels. In this case, the operation can be complicated by the fact that such a tumor is very hard and strongly "interwoven" with the surrounding area, and therefore the operation can take a very, very long time.
The position in the brain can also be very difficult. For example, I can remember a cavernoma - which is a vascular malformation - that was located in the thalamus, really very, very deep in the brain. In that case, the choice of the optimal access was the first big challenge. I decided in that case to operate via the opposite side of the brain through the cortex, the opposite lateral ventricle, then an approach to the third ventricle and adjacent to that the cavernoma. That's also a challenge because the fornices are in the way. These are the structures through which memory content is generated. In the case of bilateral damage, this means that the patient* would not be able to remember any new information. This would mean severe brain damage.
Herniated discs in the thoracic region (intradural thoracic disc herniations) can also be very challenging. This is a completely different condition than herniated discs in the cervical or lumbar spine. They can be huge, narrow the spinal canal (the space where the spinal cord is located) by over 90%, and also have massive calcification, like small limestones. These herniated discs develop over years and can also penetrate through the hard meninges. They are often located in front of the spinal cord, which means that they cannot be operated on from the back, but must be passed through the thoracic cavity. This involves removing part of the vertebral body above and below it and the intervertebral disc. Then this rock-hard space must be removed from the spinal canal and the spinal cord skin, and folded away from the spinal cord - which is thinned to one-tenth due to the herniated disc - without causing additional damage to it, because otherwise the patient would be paraplegic. Thoracic disc herniations, however, occur much, much less frequently than disc herniations in the cervical or lumbar spine. Finally, the watertight replacement of the hard meninges at this site can then be quite challenging.
Prof. Dr. med. Stoffel: Really difficult operations can sometimes take more than 12 hours. You have to develop your own techniques for getting through the operation and resting in between so that you don't become impatient late in the procedure due to fatigue or similar.
Prof. Dr. med. Stoffel: Even with glioblastomas, there are a number of factors that improve or worsen the prognosis (i.e., the time until the tumor returns and life expectancy). Since we know more about glioblastoma from molecular biology, we know: not every glioblastoma is the same. That's one point. The second point is that depending on the location, depending on how radical (i.e., as complete as possible) one can operate, and depending on the general condition and age of the patient, large differences are also possible nowadays. The third point is that more and more treatment options have been added in recent years.
Since I started in neurosurgery, a lot has changed in the treatment of glioblastoma. In the past, less emphasis was placed on removing this tumor as completely as possible, knowing that early in the disease process individual cells migrate far beyond the visible tumor into the apparently still healthy brain and deducing from this that radical surgery would do little to change the poor prognosis. Apart from surgery, there used to be hardly any other options to prevent or slow down the growth of tumor cells remaining in the brain - only radiation.
It wasn't until less than 20 years ago that another important milestone in improving the prognosis of this disease came in the form of a chemotherapy called temozolomide.
For about seven years now, there has been another - scientifically proven - very effective component in glioblastoma therapy: tumor-treating fields (TTF for short). In this procedure, so-called optodes are applied to the head, creating a magnetic field in the brain, which disrupts the cell division of the glioblastomas and causes the dividing cells to die.
There has also been a paradigm shift with regard to the surgical procedure: Nowadays, attempts are made to remove glioblastomas as completely as possible (supramarginal), i.e., beyond what can be seen on MRI. For this purpose, the glioblastoma cells are marked intraoperatively with fluorescent dye, which is drunk by the patient preoperatively, and the tissue that accumulates fluorescent dye is also removed during surgery, if this is functionally possible. This procedure also improves the prognosis. There has also been a lot of learning in the last 20 years about how to be as functionally gentle on the brain as possible while still operating as aggressively as possible on the tumor.
This includes, among other things, neuronavigation, with which a target can be reached with pinpoint accuracy - even without direct visual control. In addition, intraoperative neuromonitoring now plays a very important role in cranial surgery (surgery in the brain). This involves constant monitoring of the pathways of individual brain functions, such as the motor pathway, during tumor resection. This allows the surgeon to remove a tumor that lies directly on or even in the motor pathway as completely as possible while sparing the function as much as possible. Functional monitoring of the speech center has also become common. These procedures are called awake craniotomies because the function speech is checked with the assistance of the awake patient. This means that the patient speaks under the guidance of a speech therapist during the operation. Individual areas are stimulated again and again with the question of whether a speech disturbance occurs due to the stimulation, in order to find out where tissue can be removed and where not.
With all these changes, some major and some minor, in recent years, a life expectancy of two years and more is now quite feasible for glioblastomas. But unfortunately not in all patients, there are patients who develop a recurrence very early - that is, a tumor that grows back - which can no longer be operated on. But there is also a growing awareness of the benefits of second and third surgeries for glioblastomas located in brain areas where surgery is functionally safe.
Prof. Dr. med. Stoffel: For many diseases, the results have become much better because we know more about the individual diseases and therefore know more precisely that it is also worthwhile to operate very precisely or aggressively - even if the tumor recurs. On the other hand, we have gained many additional measures that can be of great advantage in individual cases, such as stereotactic radiosurgery (Gamma-Knife or Cyber-Knife) or also particle irradiation/proton irradiation to keep a tumor in check in a function-preserving or function-saving way. I had addressed the chemotherapeutic agents, and the tumor therapy fields as well. For metastases in the brain, there have been very significant improvements with targeted therapies with specific drugs, such as immunomodulators.
When I started in neurosurgery, a patient who had a metastasis from a peripheral tumor was actually doomed to die. It was known, completely without treatment, he had a life expectancy of about one month due to the brain metastasis, with radiation only, about three months, and with surgical removal and post-radiation, it got a little bit longer. Nowadays, we often see these patients for years after we remove a metastasis from them in clinically excellent condition. Down the road, another metastasis may be treated with gamma knife, then again the original treating specialist oncologists treat again with an immunomodulator and so these patients can often be treated in good functional condition and with good quality of life for years with very good quality of life. There's been an insane amount of progress on a lot of different levels.
Prof. Dr. med. Stoffel: Let's look at the issue of knowledge transfer. That is something that is definitely different nowadays than it was 30 years ago. Nowadays, when a well-done study comes to a successful conclusion, it is published. This publication at a medical congress or in a medical journal is immediately available to everyone, so that anyone in the world who can afford this medical technique or this drug, believes in it and wants to introduce it in their own house, can then adopt it very quickly. So that it is often a question of money and scientific attention whether you can implement the techniques or drugs at your own site, rather than a question of where in the world it was developed and first applied. Knowledge transfer today is extremely fast, so one would actually assume that in all well-resourced and also science-believing regions, primarily in the Western world, but also in the Asian region, a treatment that has been shown to be useful and better than the previous treatment would be quickly adopted. Here at Helios, we also have specialist groups and working groups in which physicians in a specific field meet regularly to evaluate new developments and decide on their use in Helios clinics.
Prof. Dr. med. Stoffel: You don't really do classical experimental treatments of an oncological nature. If there is a new procedure or a new drug, it would initially be used exclusively in the context of scientific studies. University hospitals are usually the primary treatment leaders here, but we as maximum care providers also participate in such studies. In this setting, if you will, experimental measures are compared on an ethically defensible level against gold standard measures (i.e., the currently available, proven, best possible treatments). We do not perform purely experimental measures because we do not feel, via study of the literature over the past 30 years, that this provides more benefit than risk to the patient and therefore do not consider it ethically defensible.
Prof. Dr. med. Stoffel: The following specialties are always present: in addition to neurosurgery, this includes neuroradiology, neurology, oncology, radiation therapy and colleagues from gamma knife (i.e. stereotactic radiosurgery). The idea of an interdisciplinary board is that some diseases are so complex that only as a team can we adequately evaluate what is the best option for the individual patient.
This is not the case for all patients. Often, treatment can follow a standard regimen, but sometimes it is very important. You have to know: On all of these subtopics, the literature knowledge or the literature opinion is constantly changing, and that's why these interdisciplinary boards are important. In addition, with the many different new immunomodulators, the weighting between the individual measures is also changing rapidly.
Prof. Dr. med. Stoffel: This is a very double-edged sword. For example, there are these "manager screenings" where whole-body scans are performed at regular intervals. Of course, in individual cases, you may have a chance of detecting a disease earlier in the process, long before it becomes symptomatic, such as a (low-grade) glioma. But one must be aware of the fact that many findings can be made in the body which then cause concern, but which may remain completely asymptomatic for a lifetime and with which the patient then has to deal on the basis of what is actually a baseless examination.
There are also processes in the brain, such as brainstem cavernomas or other large vascular malformations, that can be an extreme emotional burden when one learns of them. Findings that may never become symptomatic. There is no recommendation in the scientific societies or even in the guidelines for whole-body scans without any reason in my specialty.
Prof. Dr. med. Stoffel: In my opinion, the biggest challenge is consistency, and I tell that to all my residents and young attendings. It's not done with celebrating short-term successes or noticing short-term improvements in yourself, but consistency in quality is insanely important. This requires a very continuous discipline, without which you are not and will not remain a good neurosurgeon.
I was at the theater with my family and there were jugglers and equilibrists on stage. Then I thought to myself: This is an unusual activity. They first have to bring something to perfection, then they can do this activity safely and then they have to show this perfection again every evening. It's no use that they were able to do it last week. They have to be able to do it perfectly again every night. Then I noticed the analogy to my field: It's no use being able to basically remove an aneurysm or an angioma or a tumor from the speech center or the spinal cord. You have to do it successfully every time, and it is always the performance of that one time that counts. This example perhaps vividly represents how subtle neurosurgery is.
Prof. Dr. med. Stoffel: What I just described is a major part that fascinates me. Also, of course, I'm fascinated by the organs we work on - especially the central and peripheral nervous systems and their sheaths. It is of ultimate importance to us as individuals. I am also fascinated by the clearly recognizable quality of results. You can't pretend that everything went optimally if the patient has neurological dysfunction after surgery. Similarly, if you treat a patient with a degenerative spinal disease and he still has severe pain at the end. Then you have to admit to yourself: Something about the whole process was not optimal; either the indication or the way you did the treatment.
Ultimately, the ethics of medical practice play an important role. Practicing medicine is not just a service, it is caring for someone with the goal of improving their condition.
Read more:
Do you need more information about Helios Hospitals or want to schedule your treatment?


